PATELLAR INSTABILITY
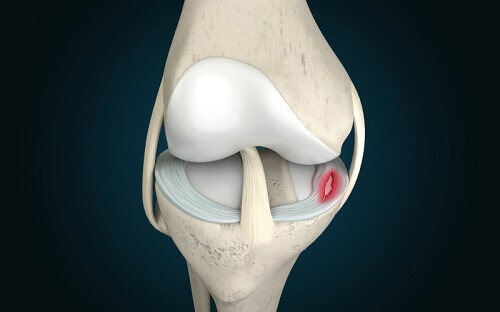
The knee can be divided into three compartments: patellofemoral, medial and lateral compartment. The patellofemoral compartment is the compartment in the front of the knee between the knee cap and thigh bone. The medial compartment is the area on the inside portion of the knee, and the lateral compartment is the area on the outside portion of the knee joint. Patellofemoral instability means that the patella (kneecap) moves out of its normal position. This malalignment can damage the underlying soft structures such as the joint surfaces, and the ligaments that hold the patella in place.

- Causes
- Symptoms
- Diagnosis
Patellofemoral instability can be caused because of variations in the shape of the patella or the opposing surface (trochlear groove). Normally, the patella moves up and down within the trochlear groove whilst the knee is bent or straightened. Patellofemoral instability occurs when the patella moves either partially (subluxation) or completely (dislocation) out of the trochlear groove.
A combination of factors can cause this abnormal tracking and include the following:
Severe leg malalignment, for instance ‘knocked knees’, or torsional deformity (inward or outward twist of the thigh or shin bones).
A ‘high’ patella (‘Patella Alta’), whereby the kneecap is located above the trochlea groove and can move to the outer side easily.
A twisting injury or acute trauma to the inner aspect of the knee (this may push an already unstable kneecap out of place).
Patellofemoral instability causes loss of confidence – a feeling that the knee may buckle or give way, typically when turning or twisting. When the kneecap slips partially or completely you may have severe pain, swelling, bruising, visible deformity and loss of function of the knee.
Your doctor can usually make the diagnosis through your history and the physical examination. Diagnostic tests such as X-rays, MRI and CT scan will give information on the presence of any of the underlying developmental predisposing factors, and the presence of secondary damage to the cartilage surfaces of the knee.
Conservative Treatment
If the kneecap has been completely dislocated, the kneecap may need to be repositioned back in its proper place in the groove. This usually happens in an emergency room under sedation. This process is called closed reduction.
The initial treatment of patellar instability is nonsurgical, comprising of pain medications, rest, ice and physical therapy to regain movement, and optimise the muscular control of the patella. Knee bracing may have a role during high risk activities.
Surgical Treatment
If the instability continues, then surgery may become necessary, both to reduce the symptoms associated with instability, and to prevent damage to the joint surfaces in the long term.
In general the surgery may be either directed at the soft tissues alone, reconstructing the ligament on the inner side, or adding a bone operation whereby the attachment of the patellar tendon on the tibia is moved towards the inner side. Both procedures improve alignment and tracking. The examination and preoperative imaging will guide whether both are appropriate, and your surgeon will discuss these with you.
Post Operative Care
Your doctor will recommend pain medications to relieve pain. To help reduce the swelling you will be instructed to elevate the leg and apply ice packs over the knee. Crutches and a hinged knee brace are necessary, depending on which operation you have had. The rehabilitation will be supervised by expert physiotherapists.
Risks & Complications
The operation is effective in the majority of cases. The risks are low but may include:
- Stiffness
- Recurrent instability (10%)
- Persistent pain and weakness of the quadriceps muscle